
What is PVD ?
This is a disease of the peripheral blood vessels ( legs or hands ) that is commonly caused by deposition of cholesterol and fatty substances. This reduces blood supply to the feet and causes specific symptoms.
What are the symptoms of PVD ?
The symptoms can be varied, depending on the degree of reduction in blood supply and can be :
? Skin discoloration, darkening or dryness of skin.
? Pain on walking or exercise ( claudication ).
? Pain at rest.
? Small non healing ulcers on toes / feet.
? Large non healing ulcers on feet.
What the risk factors for PVD ?
Smoking, diabetes, lack of exercise, heredity, high blood pressure, concurrent heart disease.
What are the tests that can help detect this disease ?
A clinical examination where a doctor feels for the feet arterial pulses and a colour Doppler ultrasound examination can help in detecting peripheral vascular disease. Other tests like a CT Angiogram or a MR Angiogram can also detect PVD as well as help in treatment planning.
What are the non surgical options that can help treat this condition ?
Early PVD can be treated by lifestyle modification measures like stopping smoking, regular exercise, obesity management, controlling diabetes, reducing serum cholesterol levels and anti platelet and cholesterol lowering medications.
What are the Minimally Invasive options available ?
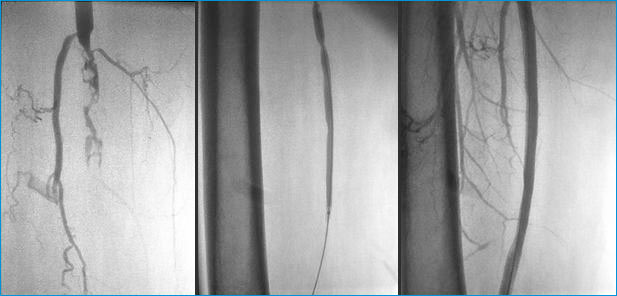
Angioplasty and stenting can treat most arterial occlusions. In this procedure, a small needle puncture is made at the groin to gain access to the vascular tree. Small instruments like catheters and wires and contrast material are used to quantify the length and degree of the blockage and then these are treated by either balloon angioplasty alone or by angioplasty and stenting. human hair wigs
Can you describe a routine angioplasty and stenting procedure from the patient’s point of view ?
Sure, when you do decide to get an angioplasty and stenting done, you would be put on dual antiplatet medications and asked to come early in the morning, around 9 am on an empty stomach.You would then be admitted in the hospital and a nurse would explain the procedure would again be explained to you. Your medications would be confirmed. An attendant will shave and prepare your groin area. You can do this at home before coming to the hospital, to avoid embarrassment.
You would then be rolled into the Cath-Lab holding area, where an IV line would be placed. Now, you would be taken inside the Cath-Lab and placed on the table. The operating doctor ( an Interventional Radiologist ) would then localise the femoral artery on the opposite side of the affected leg and then give you a small local anaesthetic injection to numb the area (over your groin). A vascular sheath would be placed into the common femoral artery and an angiogram will be performed. The lesion would be localised and quantified. The sheath would then be replaced with a cross over sheath. This is a longer sheath that would reach the opposite side and would make access to the affected leg easier and also facilitate the exchange of catheters, wires and balloons. The lesion would then be treated using an appropriately sized balloon and stented ( If required ). The vascular sheath would then be removed and the access site closed using either manual compression or a closure device like Angioseal.
You would then be transferred to your room. Immobilization of your legs is mandatory for the next 4 hours, to prevent any bleeding from the access site.
You would be put on low molecular weight heparin injections for the next 4 days and will be asked to continue antiplatelet medications.
You would be discharged the next day of the procedure.
What are the possible complications of the procedure ?
Bleeding from the access site, haematoma formation, arterial rupture, distal thrombo-embolism are some complications that can occur. We take all precautions to prevent these from occurring, but if any do occur, our trained Interventional Radiologists can competently treat them.